Shunting and Ventriculostomy
Why is this surgery done?
Hydrocephalus is a condition in which excess cerebrospinal fluid (CSF) builds up within the ventricles of the brain. The ventricles are fluid containing cavities deep inside the brain. Hydrocephalus is caused by a mismatch of CSF production and absorption. This, in turn, causes an increase in pressure within the brain.
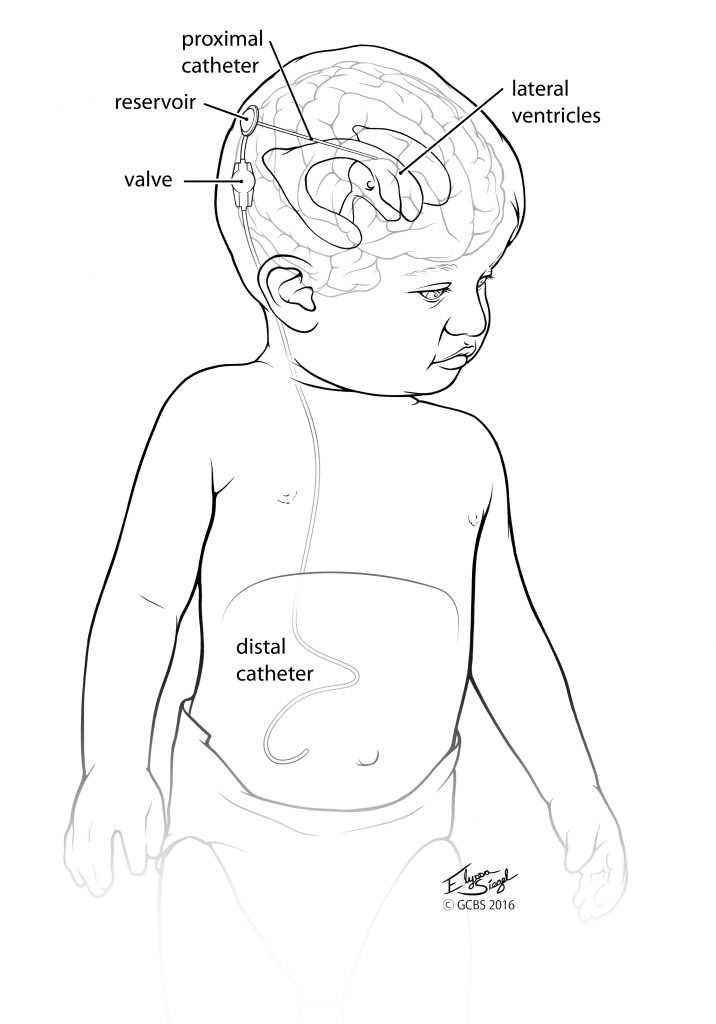
A shunt is a surgically implanted device used to help manage hydrocephalus. It drains the extra CSF from the ventricles in the brain and places it into the abdominal area or right atrium of the heart in order to relieve pressure on the brain.
Another procedure for the treatment of hydrocephalus is an endoscopic third ventriculocisternostomy (ETV). ETV allows CSF to bypass the obstruction causing the hydrocephalus and circulate from the ventricles to the space surrounding the brain so that it can be reabsorbed back into the vascular system.
How is the surgery done?
The surgery is performed by a pediatric neurosurgeon in the operating room. Your child will be asleep for the surgery. A catheter (tube) is placed into the ventricle in the brain using a navigation system to make positioning of the catheter in the ventricle as safe and accurate as possible. This tubing exits through a hole made in the skull, known as a burr hole. It is attached to a reservoir or valve that is situated outside the child’s skull but under the skin. The valve is then connected to additional shunt tubing under the child’s skin, which is tunneled down to an appropriate drainage site. This creates a continuous CSF drainage system.
The most common drainage site is inside the belly in the abdominal area known as the peritoneal space. Another safe site for drainage is the right atrium of the heart. The right atrium is used as a drainage site if the belly is not a good option. Once the shunt is placed, your child will typically require the shunt for their lifetime.
Alternatively, if your child has a high ETV success score he/she may be offered an ETV as a means of treating the hydrocephalus. ETV involves making a burr hole in the skull and with the help of a small scope or camera the neurosurgeon is able to make a small hole in the floor of the ventricle. This allows CSF to bypass the obstruction causing the hydrocephalus and restores the circulation of CSF from the ventricles to the space surrounding the brain so that the CSF can be reabsorbed back into the vascular system.
What are my risks? What are common complications?
Risks of shunt placement include but are not limited to:
- Infection
- Bleeding
- Leaking of CSF or swelling around the shunt valve or tubing
- Bruising along the neck, clavicle or chest due to tunneling of the shunt
- Shunt malfunction or infection
Shunts can fail or become infected. Signs and symptoms of shunt malfunction and infection must be monitored closely throughout your child’s lifetime. Some of the signs and symptoms of a problem include but are not limited to:
- Headaches
- Nausea/vomiting
- Lethargy (sleepiness)
- Irritability
- Abnormal vision changes
- Tense, bulging “soft spot” or prominent scalp veins
- Swelling or redness along the shunt tract
- Abdominal pain
- Fever
Complications from ETV surgery include but are not limited to:
- Headaches/nausea/vomiting for hours to several days after surgery
- Bleeding — can be severe with basilar artery injury
- Infection
- CSF leak
- Fever
- Neurological complications including weakness, memory disorder and altered consciousness
- Endocrinologic abnormalities — diabetes insipidus, weight gain, precocious puberty
- Electrolyte imbalances
- Visual field deficit
- Failure of the ETV with need for shunt placement
What do I need to know before surgery?
Prior to surgery, a head CT scan will be obtained to allow the pediatric neurosurgeon to see the brain and ventricles and determine the best position/entry site for the ventricular catheter or to guide the ETV.
The family will receive communication at least two days before coming to the hospital about where to go the day of surgery, as well as specific instructions regarding home medications and when to stop eating and drinking prior to the surgery.
Expect to spend 1 – 2 days in the hospital after surgery. Your child will be admitted to the general pediatric floor, where they will be monitored closely. Pain medication will be given as needed to ensure maximum comfort for your child. Our goal is to maintain the utmost safety, comfort and healing of your child.
The pediatric neurosurgery providers at Goodman Campbell Brain and Spine are specially trained on this diagnosis and are experts in the care of hydrocephalus. We know it can be a scary time, and we have a team of medical professionals who are available to answer any questions or discuss any concerns that you might have.
General discharge instructions
If skin glue was used on the incision, expect it to fall off in 2 – 3 weeks. Do not apply oils, lotions or creams to the glue or surrounding area. Do not allow your child to peel or pick at the glue or the incision.
If the incision is covered with a bandage, it may be removed five days after the surgery. The bandage may be left off if the incision is dry. Please keep it covered if your child is touching or picking at the incision.
If non-absorbable sutures were used, they will be removed in our office 2 – 3 weeks after surgery.
Your child may bathe five days after surgery, but do not submerge the incision until it is scab-free and looks like a scar.
Over-the-counter medications such as ibuprofen and Tylenol are recommended for pain control.
A prescription for narcotic pain medication will be sent home for your child to be used as needed for moderate pain. Most children only need a few doses of prescription pain medication at home before pain is able to be well controlled with over-the-counter medications.
Restrictions include:
- No lifting over 5 – 10 pounds (a gallon of milk weighs five pounds)
- No activities that stretch or put pressure on the incision
- No contact activities until cleared at your follow-up appointment
What should I expect while recovering?
Your child will spend 1 – 2 nights in the hospital before going home. Most children only need a few doses of prescription pain medication at home before pain is well controlled with over-the-counter medications. Your child should be able to return to school about one week after surgery. We will see your child in clinic for a follow-up 2 – 3 weeks after surgery and then again three months after surgery.
Call the neurosurgeon’s office if at any time your child experiences:
- Redness, swelling or drainage at the incision site
- A fever greater than 100.5 degrees F
- Pain not well-controlled with pain medications
- Difficulty with bowel or bladder function despite stool softener and laxatives
- Any of the signs or symptoms of a shunt malfunction mentioned above
Treatments
Request an appointment online and we will guide you through the next steps
Get to know the physicians of Goodman Campbell
Goodman Campbell
Patient Stories
Request an appointment online and we will guide you through the next steps.
