Sciatica: What Is It? – An Introduction
Millions of people each year find themselves searching for answers about sciatica symptoms and how best to pursue effective sciatica treatment. Whether your pain has just begun or you’ve been struggling for months, you are not alone. Sciatica affects people from all walks of life, often causing discomfort and concern that can impact their everyday routines, relationships, and peace of mind.
Understanding sciatica is an empowering first step on your path to healing. When you know what to expect, you can make informed decisions about moving forward. Sciatica is more than a diagnosis; it’s a journey that so many families and individuals, just like you, have faced and overcome, sometimes with the help of compassionate medical experts and tailored care plans.
This article is designed to walk alongside you and your loved ones as you seek clarity and solutions. We’ll explore what sciatica is, how common it is, and most importantly, what you can do about it. We’ll also cover the symptoms you should watch for, the variety of treatment approaches, and how you can find immediate relief or long-term recovery. The goal is to give you confidence, restore hope, and illuminate the next steps on your journey to comfort and healing.
Why Understanding Sciatica Matters
When you clearly understand the symptoms and treatment options available for sciatica, you become your own best advocate. Early recognition of sciatica and knowing when to seek help can make a significant difference, potentially preventing further complications and minimizing disruptions to your daily life. By embracing knowledge, you can find strength, comfort, and the tools needed to regain your mobility and well-being.
If you ever feel uncertain or overwhelmed, remember that you deserve answers and effective care. Don’t hesitate to ask your doctor about Goodman Campbell, where hope and expert guidance are always within reach.
What Is Sciatica?
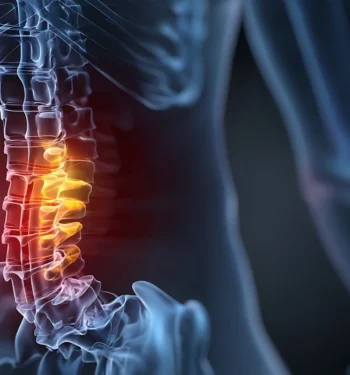
Sciatica refers to a type of pain that follows the path of the sciatic nerve, the largest nerve in the body. This nerve runs from your lower back, through your hips and one buttock, and continues down the back of each leg. Sciatica is not merely general back pain; it is a specific type of nerve pain that often generates specific, recognizable symptoms. Importantly, sciatica is a symptom caused by an underlying medical condition, such as a herniated disc or spinal stenosis.
Understanding basic anatomy is essential for anyone seeking relief from sciatica symptoms. The sciatic nerve is made up of several nerve roots that emerge from the lower sections of the spine (the lumbar and sacral spine). These roots bundle together in your lower back, moving through the buttocks and down each leg. When any part of this pathway becomes compressed — whether from a herniated disc, bone spur, or another cause — the result can be pain, tingling, numbness, or weakness that radiates from the lower back down the leg. This specific pattern helps differentiate sciatica from other forms of back or muscle pain.
What Makes Sciatica Different From General Back Pain?
While many people experience lower back discomfort at some point, sciatica stands out due to its unique symptom pattern. Sciatica is different from general low back pain, which may not radiate down the leg. Instead of generalized ache or stiffness, sciatica symptoms tend to follow the pathway of the sciatic nerve, moving outward from the lower back through one buttock and down the leg. Sciatica can cause pain, numbness, or weakness that may extend down to or involve the knee, sometimes affecting mobility and sensation. This is often described as a sharp, shooting pain, sometimes accompanied by a burning sensation, tingling, or even weakness in the leg or foot. Unlike muscular back pain, sciatica often gets worse when sitting or with certain movements, such as coughing or sneezing.
Why Is Proper Identification of Sciatica Important?
Because sciatica is rooted in nerve problems rather than muscular strain, treatment approaches differ. Properly identifying the condition allows healthcare providers to target therapies and medications that specifically relieve nerve pain and address underlying causes, such as disc herniation or nerve impingement. If left untreated or mistaken for a less serious issue, sciatica can worsen, sometimes leading to chronic discomfort or even permanent nerve damage.
Recognizing the signs of sciatica and differentiating it from other types of back pain are a vital first step toward lasting relief and recovery. If you’re experiencing pain radiating down your leg, along with numbness or tingling, don’t hesitate to seek professional help. For compassionate, comprehensive care, request an appointment at Goodman Campbell and start your journey toward healing and hope.
How Can I Tell if My Pain Is Sciatica?
Sciatica is often confused with other types of back or leg pain, but there are specific symptoms that can help you identify if what you’re experiencing is truly related to the sciatic nerve. Typically, sciatica pain follows a unique pattern, radiating from your lower back, through one buttock, and down the back of one leg. Sciatica pain can also affect the lower leg, leading to symptoms such as numbness, weakness, or tingling in that area. Recognizing these sciatica symptoms and understanding how they differ from other pain sources is essential for seeking the right treatment and achieving lasting relief.
What Does Sciatica Pain Feel Like?
Sciatica is usually described as a sharp, shooting pain that travels from the lower back, through the hip and buttock, and down the side or back of one leg. Some people note a feeling like an electric shock, while others experience burning, tingling, or even numbness along the same pathway. Swelling around the sciatic nerve or affected tissues can also contribute to pain and discomfort. The pain can be constant or may come in waves, often worsening when you’re sitting, coughing, or sneezing.
Key Symptoms That Distinguish Sciatica
Unlike general back pain, which is often limited to the lumbar area, sciatica typically impacts only one side of the body and can extend all the way down to the foot. You may notice muscle weakness in the affected leg, difficulty moving your foot or toes, or a pins-and-needles sensation. Sciatica can also affect your ability to perform daily activities due to pain, numbness, or weakness. These patterns are strong indicators that your pain could be caused by pressure or irritation of the sciatic nerve and not by a simple strain or muscle pull.
The Importance of Proper Diagnosis
Receiving a proper diagnosis for sciatica symptoms is crucial. Many other conditions, including joint issues, vascular problems, and localized injuries, can mimic sciatica. A healthcare provider may use a physical exam, your symptom history, and sometimes imaging tests to confirm the diagnosis. This ensures you get a treatment plan tailored to address the root cause of your discomfort, not just the symptoms.
When Should You Seek Medical Evaluation?
If your pain is persistent, gets worse, or is accompanied by other concerning symptoms such as loss of feeling, muscle weakness, or trouble controlling your bladder or bowels, it’s time to seek professional care. If you are unsure whether your symptoms are sciatica, consult your primary care provider for an initial evaluation and guidance. Finding the right team is key. Ask your doctor about Goodman Campbell for access to specialists who are experienced in both nonsurgical and advanced interventional treatments for sciatica. We can help you find your path back to the activities you love.
What Are the Main Causes of Sciatica?
The main cause of sciatica is pressure or irritation of the lumbar or sacral nerve roots, which connect to the sciatic nerve, most commonly due to a herniated disk in the lower back. A herniated disk is a common cause of sciatic nerve compression, leading to inflammation, pain, and numbness in the leg. Other significant causes include spinal stenosis, bone spurs, and, less commonly, infections, tumors, or trauma. There are also conditions affecting the small bowel, colon, rectum, and pelvic floor that may require specialized care if they contribute to sciatic symptoms. Understanding what leads to sciatica can empower you or your loved ones to seek timely, effective care and make informed decisions about treatment and recovery options. Read on to explore these potential causes and related conditions in detail so you can better recognize and address the root cause of your pain.
What are the most common causes of sciatica?
The most frequently occurring cause of sciatica is herniated disks, where the cushioning material between your spinal bones slips out of place or ruptures, pressing directly on the nerve roots that form the sciatic nerve. In many cases, herniated disks causing sciatica improve without the need for invasive treatment, as natural recovery is common in many cases. This direct nerve compression can trigger pain, numbness, and weakness radiating from your lower back to one side of your buttocks and down your leg. Conditions such as spinal stenosis — when the spinal canal narrows and puts pressure on nerves — and bone spurs from arthritis also frequently cause sciatica.
How do degenerative spine diseases contribute to sciatica?
Degenerative spine diseases, including osteoarthritis and degenerative disc disease, gradually wear down spinal structures. As discs lose moisture and collapse, or as joints become inflamed and develop bone spurs, the resulting narrowing of pathways in the spine can press on nerve roots. This chronic process can turn mild back discomfort into persistent, sometimes severe sciatica buttock pain that interferes with walking, sitting, or enjoying the things you love.
What are less common causes of sciatica?
In rare instances, sciatica may be caused by acute injury, such as falls, fractures, or significant trauma, which can result in nerve or musculoskeletal damage leading to sciatica. Inflammation or infection in the area surrounding the sciatic nerve can also mimic classic sciatica symptoms. Even the sacroiliac (SI) joint — where your spine meets your pelvis — can become inflamed (a condition called sacroiliitis) or irritated and cause a similar pattern of buttock or leg pain, often referred to as radiculopathy if nerve roots are involved.
How are SI joint pain and radiculopathy related to sciatica?
The SI joint connects your spine to your pelvic bones. When inflamed, it can irritate nearby nerve roots, triggering symptoms that closely resemble sciatica — sharp, radiating pain through one side of the buttocks and down the leg. Radiculopathy refers more broadly to any condition in which a spinal nerve root is compressed. Diagnostically, sciatica is a type of radiculopathy affecting the lower spinal nerves. Recognizing these overlaps helps doctors pinpoint the precise origin of your pain and provide more specialized care.
If you or someone you care for are experiencing persistent lower back or buttock pain that radiates down the leg, don’t wait for the discomfort to take over your daily life. Early intervention can make a remarkable difference in recovery and well-being. Remember to ask your doctor about Goodman Campbell to get an expert diagnosis and compassionate care tailored to your needs.
What Are Common Symptoms of Sciatica?
Sciatica symptoms often manifest as pain that radiates from your lower back, through one side of the buttocks, and down the leg. While the severity and nature of this pain can vary widely from person to person, it commonly presents as a sharp, burning, or shooting discomfort that dramatically interferes with daily life. Recognizing these symptoms early can be empowering, helping you to understand what’s happening in your body and guiding you toward the right care.
What are the common symptoms of sciatica?
Classic sciatica symptoms include a distinct pain that follows the pathway of the sciatic nerve. This often starts in the lower back or one buttock and travels down the back of the thigh and calf, sometimes reaching as far as the foot. The pain can range from a mild ache to a sensation so severe it feels like an electric shock. For many, the pain intensifies when sitting, coughing, or sneezing, and it can make movement or walking especially challenging.
Can sciatica cause numbness or weakness?
Yes, beyond just pain, sciatica may also cause sensations such as numbness, tingling, or even a pins-and-needles feeling in the affected leg and foot. Some individuals experience muscle weakness, which might make it difficult to lift the foot (a symptom called “foot drop”) or perform everyday activities such as climbing stairs or standing.
Why does sciatica pain worsen with movement or sitting?
Activities that put additional pressure on the nerve, such as prolonged sitting, moving from a seated to standing position, or even certain movements like bending or twisting, can make pain worse. Certain positions, such as lying with pressure on the buttocks, can also increase sciatic nerve discomfort. This happens because the sciatic nerve can be compressed or irritated by spine conditions like herniated discs or bone spurs, and any action that narrows the space in the spine may exacerbate symptoms.
When do symptoms of sciatica indicate a medical emergency?
Although most cases of sciatica gradually improve, certain symptoms should never be ignored. If you experience sudden loss of bladder or bowel control, significant weakness or numbness in the legs, or pain that is so unbearable you cannot walk, it may signal a serious underlying problem. In such cases, you should seek immediate medical attention. These could be signs of nerve damage or cauda equina syndrome, which require urgent intervention.
Understanding and recognizing these sciatica symptoms gives you the power to seek help proactively. If you identify with any of these symptoms, or if your pain is holding you back from living the life you love, request an appointment at Goodman Campbell. Our caring specialists can guide you toward effective solutions, helping you reclaim your mobility and rediscover hope for a more active, comfortable life.
What Is the Best Treatment for Sciatica?
Finding the best treatment for sciatica is a journey tailored to each individual’s needs, symptoms, and underlying causes. The goal of treatment is not only to relieve pain but also to treat the underlying cause of sciatica. Sciatica treatments range from simple self-care and medication to advanced procedures, and recovery is possible with the right support. Let’s explore proven treatment pathways that have been shown to bring relief for many patients.
What Nonsurgical Options Are Available?
For many patients, nonsurgical sciatica treatment is often the first line of care and brings meaningful relief. Simple measures such as rest, gentle stretching, heat and ice application, and short-term activity modification can help reduce inflammation and muscle tension. Guided physical therapy is foundational, strengthening core muscles, improving flexibility, and teaching proper ergonomics to prevent future flare-ups. It’s important to stay as active as your symptoms allow to encourage healing, but always under the guidance of your care team.
Which Medications Relieve Sciatica Pain?
When pain prevents normal activities, over-the-counter medications may ease discomfort. For more severe episodes, your provider may suggest prescription medications to target nerve-related pain. Although medications can often provide immediate relief for sciatica pain, their use should be tailored and monitored closely by your doctor to avoid side effects and dependency. It is also important to discuss potential drug interactions with your doctor when starting new medications for sciatica.
What Are My Options for Interventional Pain Management?
For persistent or severe sciatica, advanced interventional procedures are available. Epidural steroid injections can deliver potent anti-inflammatory medication directly around the irritated nerve root, providing substantial relief and buying time for the nerve to heal. Nerve blocks offer diagnostic and therapeutic value, pinpointing and soothing pain generators.
Are Minimally Invasive and Surgical Treatments Effective?
If conservative sciatica treatment fails to offer relief, minimally invasive or surgical solutions may be the key to lasting wellness. Procedures such as lumbar microdiscectomy — removal of the herniated disc fragment — can dramatically relieve pressure on the nerve root. Decompression and fusion surgeries are reserved for more complex cases but can restore function and end years of discomfort. Most people recover fully from sciatica caused by herniated disks, especially with timely intervention.
What Advanced Techniques and Devices Help?
Innovative therapies, such as spinal cord stimulators, may be considered for patients whose pain persists despite standard measures. These devices modulate pain signals before they reach your brain, giving you another chance at relieving pain. Talk to your provider about whether these options are right for you.
Every journey with sciatica is unique. To understand which treatment is best for your specific situation, ask your doctor about Goodman Campbell or request an appointment today. Our expert team will listen to your story, perform a thorough assessment, and craft a personalized plan to help you walk, move, and smile again. Getting the right help means there’s hope at every step.
How Do I Get Sciatica to Go Away?
Questions abound when it comes to sciatic nerve pain. “How do I get sciatica to go away?” “Is there a cure for sciatica?” Most people with sciatica will experience significant relief with a combination of self-care, lifestyle changes, and targeted therapies. Addressing risk factors, such as poor posture or heavy lifting, can help prevent sciatica from recurring. While some cases may resolve on their own or with conservative treatment, others require ongoing management or advanced care to prevent recurrence and ensure lasting health. With the right approach and support, it’s possible to greatly reduce or even eliminate symptoms of sciatica, empowering you to live an active, fulfilling life.
Self-Care Strategies for Lasting Sciatica Relief
Taking charge of your recovery starts at home. Simple lifestyle changes can make a profound difference in reducing sciatica pain and preventing it from coming back. First and foremost, maintaining an active lifestyle with regular, gentle exercise is key. Movement helps improve flexibility, strengthen supporting muscles, and promote healing in the affected nerve areas. Regular walking, swimming, or cycling — when approved by your doctor — can all support recovery.
Pay careful attention to your posture, both when sitting and standing. Good ergonomics matter. Choose chairs with proper lumbar support, take breaks from prolonged sitting, and practice standing with your weight evenly distributed. Also, avoid heavy lifting or sudden twisting motions that could strain your back.
In addition to self-care, a variety of services, including physical therapy and pain management, are available to support your recovery from sciatica.
Stretching and Strengthening: Building a Resilient Back
Stretching and strengthening routines are typically recommended to ease and prevent sciatica. Gentle stretches targeting the hamstrings, hips, and lower back can release compression on the sciatic nerve. Core-strengthening exercises, often guided by a physical therapist, help support your spine and reduce stress on the lower back. Incorporating a daily stretching routine — even just 5–10 minutes — can help keep symptoms at bay and enhance overall mobility.
Preventing Recurrence: Lifestyle Modifications for a Healthier Spine
One of the best ways to prevent sciatica from recurring is to take a close look at your daily habits and embrace wellness. Focus on keeping a healthy weight to minimize pressure on your spine. Managing chronic conditions such as diabetes through education, regular monitoring, and healthy lifestyle choices can also help reduce the risk of developing sciatica. Learn safe techniques for lifting objects and talk to your healthcare provider about incorporating activities like yoga or Pilates, which emphasize strength, flexibility, and mindfulness. Don’t underestimate the importance of restful sleep in a comfortable position with adequate support for your back and neck.
If your job involves repetitive motions or stationary periods, make adjustments to your workspace — ergonomic chairs, standing desks, or supportive footwear can all contribute to a healthier, happier spine.
When to Seek Professional Help for Sciatica
If self-care efforts don’t bring adequate relief — or if your symptoms are severe or worsening — it’s time to partner with a healthcare professional. Persistent pain, significant weakness, or trouble with movement means your body needs expert guidance. Physical therapy, medically supervised exercise programs, and specialized treatments can all make a marked difference.
As with many health challenges, early and comprehensive intervention is the key to lasting relief and preventing chronic problems. Ask your doctor about Goodman Campbell.
Our team is here to provide the expertise, compassion, and advanced treatment options you need to live your best life.
Immediate Relief for Sciatica Pain: What Can Help Right Now?
If you’re struggling to find immediate relief for sciatica pain, it’s important to know that several strategies can bring comfort and help you regain hope in the midst of discomfort. While sciatica can feel overwhelming, there are practical steps you can take at home, as well as medical options, that may quickly ease your pain and help you move forward with greater confidence.
What Can I Do for Immediate Relief from Sciatica Pain?
For many people experiencing a sudden flare-up of sciatica, simple home remedies can help reduce discomfort. Applying an ice pack or a cold compress to the lower back or buttocks area for 15–20 minutes at a time can help decrease inflammation and numb pain. After a few days, many patients find relief by switching to heat therapy, such as a warm towel or heating pad, which can relax tight muscles around the sciatic nerve. Gentle stretching — especially hamstring and lower back stretches — can sometimes relieve pressure along the nerve, but always move slowly and stop if pain worsens.
Which Medicines Work Quickly for Sciatica?
Over-the-counter options are commonly used for immediate relief from sciatica pain. These medications can lessen both pain and inflammation. In some cases, your doctor might recommend a prescription-strength medication if initial measures aren’t effective. Remember to follow dosing instructions and discuss with your healthcare provider before trying new medications, particularly if you have other health conditions.
Are Injections or Nerve Blocks an Option for Fast Pain Relief?
For persistent or severe pain, pain-relieving procedures such as epidural steroid injections or nerve blocks can provide more significant and sustained relief. These treatments target inflammation directly at the source and can help restore mobility while you pursue longer-term solutions such as physical therapy. If you are interested in these advanced techniques, ask your doctor about Goodman Campbell and how an interventional pain management specialist’s expertise can help tailor a treatment plan just for you.
When Does Sciatica Require Urgent Medical Attention?
It’s important to recognize when self-care isn’t enough. If your pain is so intense that you can’t walk, control your bladder or bowels, or you have severe leg weakness or numbness, seek medical help immediately. These can be signs of a serious condition needing urgent intervention. For ongoing or severe symptoms, request an appointment at Goodman Campbell. Compassionate, skilled care is just a step away, and finding real relief is possible.
What Should I Do if My Sciatica Pain Is So Bad I Can’t Walk?
Severe sciatica pain that makes it difficult or impossible to walk is a clear signal that immediate medical attention is needed. While sciatica can cause varying levels of discomfort, such intense pain suggests a possible complication like significant nerve compression, which can sometimes result in long-term damage without prompt treatment. If your mobility is suddenly affected, or if you are experiencing additional serious symptoms, it’s crucial not to wait and hope symptoms improve on their own. Emergency care may be necessary to protect your health and well-being.
Recognizing Severe Symptoms and Red Flags
If you’re dealing with sciatica pain so bad you can’t walk, you may also notice alarming symptoms such as loss of bladder or bowel control, numbness or weakness in your legs or groin, or sudden, rapidly worsening pain. These are considered neurological red flags that may indicate a condition requiring urgent intervention, such as cauda equina syndrome. In these situations, seeking immediate emergency care can be life-changing, helping to safeguard nerves and preserve function.
When Is Emergency Care Necessary?
You should visit an emergency room or contact your doctor right away if you face any of the following:
- Sudden inability to walk or stand due to leg weakness
- Loss of sensation in the genitals or saddle area
- Loss of bladder or bowel control
- Uncontrollable, severe pain not relieved by medication or rest
Getting fast, expert evaluation can be the difference between a quick recovery and long-lasting complications. Remember, your health and your ability to stay active are worth protecting. Don’t hesitate if you feel something isn’t right.
What Medicines Can Relieve Sciatica Pain?
Effective relief from sciatica pain often involves the use of medications that target both inflammation and nerve discomfort. A combination of over-the-counter and prescription medications can help manage pain, enable recovery, and restore your quality of life. However, the best approach is always individualized. What works for one person may not work for another, and side effects or other health considerations play a significant role in choosing the right medicine. Some medications used for sciatica pain may cause skin-related side effects, so it’s important to monitor for any changes in your skin and report them to your doctor. It’s essential to work with your physician to choose the medicines that best fit your health profile and lifestyle.
For many, medication is just one part of a comprehensive sciatica treatment plan. Sometimes, pain management procedures, such as epidural steroid injections or nerve blocks, administered by an interventional pain management physician, provide additional relief. Above all, if you’re unsure, in severe pain, or struggling with side effects, ask your doctor about Goodman Campbell. Our team offers advanced and compassionate solutions tailored to your unique journey toward healing.
When Should I See a Doctor for Sciatica?
Sciatica can be unsettling and even frightening, especially when pain doesn’t seem to improve or becomes severe. It’s important to remember that sciatica is often a symptom of an underlying medical condition, such as a herniated disc or spinal stenosis, which requires proper diagnosis and management. So, when should you see a doctor for sciatica? If your pain persists for more than a few weeks despite home care, is progressively worsening, or you notice symptoms like leg weakness, loss of sensation, or changes in bladder or bowel control, it’s time to reach out to a specialist. Consulting a team of experts ensures you receive an accurate diagnosis and personalized care needed for true relief and long-term recovery.
Persistent or Worsening Pain: Listening to Your Body
Most episodes of sciatica will ease up with gentle self-care over time, but persistent or increasing pain signals the need for a medical evaluation. If your discomfort is significant enough to disrupt your sleep, impact your favorite activities, or doesn’t respond to over-the-counter medications and stretching routines, don’t hesitate to seek answers and solutions from professional support. Expert assessment can help detect underlying causes, such as disc herniations or nerve issues that may require specific treatments.
Severe Neurological Symptoms: Recognizing Emergency Signs
If you experience weakness in your leg or foot, loss of sensation, or trouble controlling your bladder or bowels, don’t wait — these symptoms could indicate a medical emergency such as significant nerve compression. In such scenarios, time is critical to prevent permanent nerve damage. Always err on the side of caution, and seek prompt care if sciatica changes how your limbs function or alters your ability to manage bodily functions.
When Conservative Treatment Isn’t Working
Home remedies, physical therapy, and medications are often the first lines of defense in treating sciatica. However, if weeks of conservative treatment fail to bring relief or your symptoms are worsening, a consultation with a spine specialist becomes essential. A thorough medical workup, such as a physical examination and advanced imaging, can clarify the cause and open doors to advanced treatment options, including targeted injections, minimally invasive procedures, or surgical solutions, if necessary.
What to Expect From a Specialist Evaluation
Meeting with a specialist, especially a caring team like those at Goodman Campbell, means you’ll not only receive a precise diagnosis but also support tailored to your condition and goals. Specialists will review your medical history, perform targeted exams, and may recommend studies such as an MRI or nerve tests. Together, you’ll create a roadmap to pain relief and restored function, built on leading-edge medicine and personal attention.
How to Book an Appointment: Take the Next Step
Taking the step to reach out for expert help is a powerful act of self-care and hope. If you or your loved one is suffering from sciatica, request an appointment at Goodman Campbell. Our multidisciplinary team is dedicated to your recovery. Your journey to lasting relief and resilience can start today with the right guidance and support. Don’t let uncertainty, fear, or persistent pain hold you back from living fully. With the right help, brighter days are ahead.
Conclusion: Finding Relief and Support for Sciatica
Sciatica can be a truly overwhelming experience, impacting your ability to enjoy everyday moments with family, pursue your passions, or even fulfill simple daily tasks. While the journey to relief might sometimes feel daunting, it’s important to remember that there are effective, proven sciatica treatments available. Many people have regained their confidence and mobility after seeking the right care. You are not alone in this challenge, and hope is always within reach.
If you’re experiencing persistent or severe symptoms, don’t let frustration or fear keep you from seeking help. From innovative nonsurgical therapies and targeted pain management strategies to advanced surgical options designed for lasting sciatica relief, today’s Goodman Campbell specialists provide a customized approach tailored to your unique condition and goals. Remember that achieving relief is not just about stopping pain temporarily—it’s about reclaiming your quality of life for the long term.
How can I find lasting relief from sciatica?
Lasting relief from sciatica begins with expert diagnosis, a personalized treatment plan, and a partnership between you and compassionate specialists who understand your needs. Whether your path includes physical therapy, minimally invasive procedures, or restorative surgery, every step is guided by the expertise and dedication of your care team. Achieving sustained comfort and confidence is truly possible, and real-life patient stories can provide the inspiration to keep moving forward.
Why is expert care important for sciatica?
Expert care ensures that your symptoms are properly identified and addressed — no two journeys to healing are the same. When you work with experienced professionals, such as those at Goodman Campbell, you benefit from the latest techniques, a wide range of treatment choices, and the compassionate support you and your loved ones need throughout the healing process. Every day, patients regain mobility, alleviate chronic pain, and find hope because they made the decision to reach out for help.
What are the next steps if I want to address my sciatica?
Your next step is to speak with your doctor and focus on finding spine specialists who put your health and future first. Don’t wait for your pain to become unmanageable; instead, take a proactive approach to recovery. Early intervention often leads to stronger results, improves overall outcomes, and sets a hopeful tone for the future.
If you’re ready to start your recovery, connect with a team that celebrates your victories and supports your challenges. Many patients have already reclaimed active, fulfilling lives after confronting even the toughest sciatica symptoms. Request an appointment or ask your doctor about Goodman Campbell today, and take the first step toward a brighter, healthier tomorrow.