Introduction: Understanding Severe Spinal Stenosis Of L4-L5
A person’s well-being is rooted in their freedom of movement, yet, for many, spinal stenosis can steal their joy and limit independence. Spinal stenosis refers to the narrowing of the spaces within your spine. This narrowing can put pressure on the nerves traveling through the spine. The most common place for this to happen is in the lower back, especially at the L4-L5 region. This specific segment, found in the lumbar (lower) part of your back, is responsible for bearing much of your body’s weight and is essential for mobility, supporting everything from gentle walks to everyday activities.
When stenosis occurs at the L4-L5 level, it can be particularly significant and life-altering. This area houses critical nerve roots that are involved in leg strength and sensation, walking, and even balance. Compression in this region often affects both sides of the body, increasing the potential for severe symptoms and, in some cases, sudden loss of function.
Early diagnosis and specialized care are absolutely essential. Recognizing symptoms early allows for timely intervention, which can help you regain quality of life or even prevent further nerve damage. If ignored, the consequences of severe spinal stenosis L4-L5 can escalate, affecting not just your mobility, but your independence and happiness as well.
For those experiencing symptoms such as persistent back pain, leg weakness, or changes in bladder or bowel control, there is a path forward. Accessing the right expertise can make all the difference. Request an appointment or ask your doctor about Goodman Campbell if you’re experiencing symptoms of spinal stenosis, and take the first step toward reclaiming your well-being.
What Are the Symptoms of Severe Spinal Stenosis L4-L5?
Severe spinal stenosis L4-L5 can lead to life-changing symptoms, making it important to recognize its warning signs early. The hallmark signs include lower back pain, radiating discomfort into the legs, and increasing difficulty with daily activities. In the most aggressive cases, this condition may affect nerve function, impacting both mobility and organ control. If you notice these severe symptoms, promptly seek a specialized spine evaluation. Your comfort, independence, and quality of life may depend on early action.
Lower Back Pain and Stiffness
A primary and often earliest symptom of severe spinal stenosis L4-L5 is persistent lower back pain. This discomfort may worsen with activity or even linger at rest, accompanied by tightness or stiffness that limits flexibility and daily tasks. Don’t dismiss chronic or sharp pain, as it may indicate progression and require targeted intervention.
Radiating Pain in the Buttocks, Hips, and Legs
Compression of the nerves at the L4-L5 region frequently causes pain that radiates from the lower back and shoots down into the buttocks, hips, and legs. This sometimes manifests as sciatica — a sharp, burning pain following the path of the sciatic nerve. The pain can disrupt work, recreation, or even a simple walk to the mailbox.
Numbness, Tingling, or Weakness in the Legs or Feet
Severe cases may present with numbness, tingling, or noticeable muscle weakness in the legs or feet. These neurological symptoms can make you feel unstable, drop objects, or have trouble judging steps and uneven ground. If left untreated, weakness and numbness may worsen, underscoring the seriousness of spinal stenosis at L4-L5.
Difficulty Walking, Standing, or Balancing
Mobility can become a challenge as severe spinal stenosis L4-L5 progresses. You may find it increasingly difficult to stand upright or walk for any length of time without discomfort. Some patients describe feeling unsteady, as if their legs are about to “give out.” Difficulty balancing is a red flag that nerve involvement may be impacting your central stability.
Loss of Bladder or Bowel Control in Extreme Cases
In the most critical scenarios, severe nerve compression at L4-L5 risks loss of bladder or bowel control — a medical emergency. This alarming sign, known as cauda equina syndrome, needs immediate treatment to avoid permanent damage and loss of independence. Never hesitate to seek help if you experience these symptoms.
Increased Symptom Intensity With Standing or Walking
People with severe spinal stenosis L4-L5 often report that symptoms intensify during walking or standing, but may improve with bending forward or sitting. This classic pattern suggests nerve compression is worsening with certain movements and positions.
For a cutting-edge clinical diagnosis and treatment, ask your doctor about Goodman Campbell. Their expert team is ready to walk you through comprehensive diagnostic options and create a treatment plan tailored just for you.
What Are the Worsening Symptoms of Spinal Stenosis?
As spinal stenosis progresses, patients can experience an escalation from mild or intermittent discomfort to severe and persistent pain, which may impact every aspect of daily life. The progression of symptoms often indicates that nerves are becoming more compressed, leading to increasing neurological deficits and, in rare but critical cases, life-threatening complications. Understanding and recognizing the signs of worsening spinal stenosis is vital for seeking timely intervention and preserving quality of life.
Can Spinal Stenosis Symptoms Progress From Occasional Discomfort to Severe Pain?
Yes, spinal stenosis often begins with mild, occasional aches but can progress to intense, relentless pain as the spinal canal becomes more narrow. This pain may radiate from the lower back to the hips, buttocks, and legs, and can severely limit mobility. Activities that once were enjoyable, such as walking or standing for extended periods, may become unbearable, making early recognition and management critical for your well-being.
Do Numbness, Tingling, and Weakness Get Worse Over Time?
Absolutely. As stenosis advances, there is often a noticeable increase in numbness, tingling, or even loss of sensation in the legs or feet. Muscle weakness may also emerge and progress, sometimes leading to conditions such as “foot drop,” where lifting the front part of the foot becomes difficult. These growing neurological symptoms are signs that the nerves are under significant pressure and require immediate medical evaluation.
What Is Neurogenic Claudication, and How Does It Affect Life?
Neurogenic claudication refers to cramping, burning, or pain in the legs that worsens with walking or standing but often improves with sitting or leaning forward. This is a hallmark of moderate to severe spinal stenosis and can dramatically reduce independence, making simple activities and errands exceedingly challenging. Over time, patients may notice they need to take frequent breaks or can walk only short distances.
Can Spinal Stenosis Lead to Emergencies Like Cauda Equina Syndrome?
Severe cases can put you at risk for cauda equina syndrome, a rare but serious condition caused by extreme compression of the nerves at the base of the spine. Symptoms may include sudden loss of bladder or bowel control, numbness in the groin area, and profound leg weakness. This is a medical emergency. If you experience these symptoms, seek help immediately. Prompt surgical intervention is often required to prevent permanent nerve damage or paralysis.
How Do Worsening Symptoms Impact Quality Of Life?
As symptoms deteriorate, daily functioning and emotional health can suffer. Persistent pain, decreased mobility, fear of falling, and strong neurological symptoms can lead to frustration, anxiety, isolation, and a sense of lost independence. It can also make it harder to care for oneself or loved ones. This is why it is so important not to ignore worsening symptoms and to seek specialized spine care.
If your symptoms are worsening, request an appointment with Goodman Campbell. Timely expert care can change your life for the better.
What Is Considered A Severe Case Of Spinal Stenosis?
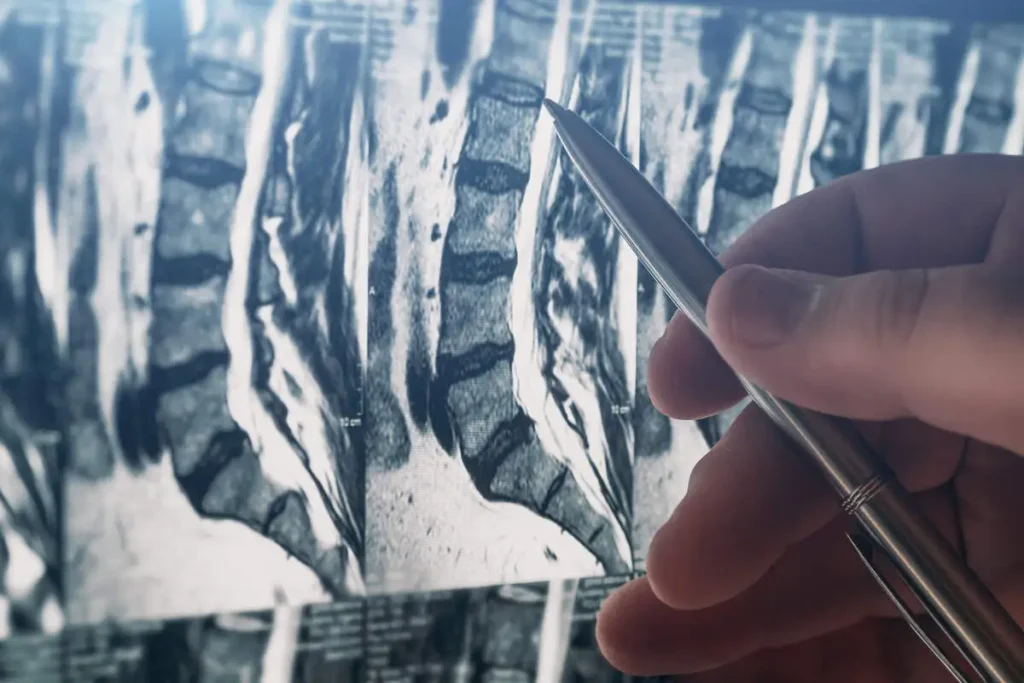
Severe spinal stenosis at the L4-L5 level is identified by both noticeable narrowing of the spinal canal seen on imaging studies, such as MRI, and the presence of significant, often worsening symptoms. This severity is not simply defined by what an X-ray or MRI shows, but also by the actual impact on daily life and the development of neurological problems like leg weakness or loss of bowel and bladder control. When symptoms persist despite attempts at conservative treatment or when neurological deficits appear, it is a strong indicator that your spinal stenosis has reached a severe and urgent stage.
How Is Severity Determined in Spinal Stenosis?
Severity is typically established through a combination of advanced imaging tests and comprehensive symptom assessment. An MRI can reveal marked narrowing of the canal at L4-L5, indicating the compression of nerves or the spinal cord. However, even with severe narrowing, not everyone experiences the same symptoms. Therefore, physicians also consider the impact on mobility, the presence of persistent numbness, tingling, or weakness in the legs, and whether bladder or bowel control is affected. Severe spinal stenosis almost always involves some degree of nerve function compromise and greatly interferes with your ability to live normally.
What Are the Signs That Spinal Stenosis Is Becoming Disabling?
Spinal stenosis at the L4-L5 level becomes especially serious when it significantly impacts everyday activities, such as walking, standing, or maintaining balance. If you find yourself unable to walk more than short distances without rest, or notice increasing numbness or weakness, these are red flags. Other severe manifestations include loss of fine motor skills, serious difficulty lifting the foot (known as foot drop), or sudden changes in bladder or bowel habits. Such changes are not just uncomfortable — they are also a sign of potential permanent nerve injury if not addressed quickly.
Can Severe Spinal Stenosis Lead to Permanent Damage?
Yes, when severe spinal stenosis is left untreated, it can lead to persistent nerve damage, disability, and a lasting loss of independence. In rare but urgent cases, compression may cause cauda equina syndrome, where rapid intervention is needed to prevent irreversible harm. This is why cases with worsening or severe neurological symptoms require immediate expert evaluation. Early intervention creates the best chance for restoring function and relieving pain.
Is Spinal Stenosis L4-L5 Serious? Absolutely. When the narrowing at L4-L5 progresses, it can severely limit your quality of life and put you at risk of major complications. If you recognize any of these signs, do not delay seeking help. Severe spinal stenosis needs the care and experience of a specialized team to properly diagnose, treat, and support you.
Request an appointment with Goodman Campbell and discover how dedicated spine specialists can help you regain your mobility and comfort.
What Surgery Is Done for Severe Spinal Stenosis in L4 and L5?
If you or a loved one is facing severe spinal stenosis L4-L5 surgery, it is completely normal to feel anxious or overwhelmed. The most common surgical options include lumbar decompression surgery, such as a laminectomy, which is designed to relieve pressure on the nerves caused by the narrowing of the spinal canal in the L4-L5 area. These procedures can dramatically improve pain levels, mobility, and overall quality of life for those suffering from the debilitating effects of severe stenosis.
Overview of Surgical Options
The gold standard for treating severe L4-L5 stenosis is often a lumbar decompression surgery. A laminectomy removes part of the bone (the lamina) that is pressing on the nerves, giving them more space and reducing symptoms, including pain, numbness, or weakness. In some cases, a micro lumbar discectomy or even a spinal fusion may be considered. Fusion may be necessary when there is instability or movement between the vertebrae after decompression.
How Surgery Relieves Nerve Compression At L4-L5
By physically creating more room around the nerves at L4-L5, these procedures significantly reduce nerve irritation and allow for better function. After surgery, many patients report feeling immediate relief from their worst symptoms and gradually return to the activities they love.
Newer and Minimally Invasive Techniques
The field of spine surgery is advancing rapidly, with the newest treatments for spinal stenosis focusing on minimally invasive procedures. These approaches use smaller incisions and specialized instruments, leading to less tissue damage, lower risk of complications, and faster recovery times. Your spine specialist can tell you whether you’re a candidate for these innovative options.
Risks and Benefits of Surgical Intervention
While every surgery carries risks, including infection, bleeding, or incomplete relief of symptoms, the benefits often outweigh these risks for those suffering from severe, disabling stenosis. Proper patient selection, careful technique, and experienced neurosurgical teams, such as those at Goodman Campbell, are essential for optimal outcomes.
Who Is a Candidate for Surgery?
Surgery is usually recommended for patients whose symptoms have not improved after conservative treatments like medication, physical therapy, or injections. It is also indicated when neurological symptoms — significant weakness or problems with walking or bladder control — become severe or progressive. Your personal goals and health will guide your care team in helping you make the right decision for you.
If you or your loved one is struggling with severe spinal stenosis at L4-L5, learn more about your advanced treatment options and request an appointment with Goodman Campbell.
Managing and Treating Severe Spinal Stenosis: What Should You Ask Your Doctor?
Managing severe spinal stenosis at L4-L5 requires a thoughtful, multifaceted approach tailored to each patient’s unique needs and level of discomfort. Patients are often surprised to discover the range of options available, from advanced pain management medications to minimally invasive surgeries and innovative therapies. It’s crucial to discuss all these options with your neurosurgeon, ensuring that your treatment plan evolves with the latest medical advancements and centers around your quality of life.
What Is the Best Way to Manage Pain Associated With Spinal Stenosis?
The first line of defense against the pain and discomfort of spinal stenosis often involves medications. Over-the-counter solutions may provide symptom relief, especially in the early stages. For more advanced pain, your doctor may consider prescription medications. Your spine specialist will help you find the safest and most effective option, taking your personal health background into account. Remember that ongoing pain deserves expert attention. Ask your doctor about Goodman Campbell to explore the best options for you.
Exploring Physical Therapy and Nonsurgical Treatments
Physical therapy remains a cornerstone in managing symptoms and enhancing mobility and strength. Skilled therapists teach specific exercises, optimize posture, and introduce strategies to relieve pressure on affected nerves. Additional nonsurgical interventions may include interventional pain management, activity modification, specialized support devices such as braces, and structured rehabilitation programs. For many patients, combining physical therapy with interventional pain management provides transformative results — restoring independence, mobility, and hope. If your current routine has plateaued, consider reaching out to a multidisciplinary team like Goodman Campbell to help you achieve better outcomes.
Embracing a Multidisciplinary Approach
Severe spinal stenosis can affect more than just your back. It can also impact your overall well-being, daily activities, and even emotional health. This is why a multidisciplinary approach is so vital for optimal healing. At Goodman Campbell, your care team may include neurosurgeons, pain specialists, rehabilitation therapists, and compassionate support staff. Together, they monitor progress, adjust treatments, and provide encouragement every step of the way. Don’t settle for fragmented care. Ask your doctor about Goodman Campbell’s holistic, team-based support for your spine health journey.
For the latest and most effective treatments in managing and treating severe spinal stenosis, request an appointment or ask your doctor about Goodman Campbell, and take the next step toward a healthier, more active life.
Conclusion: Take Action if You Have Severe Spinal Stenosis L4-L5
Living with severe spinal stenosis L4-L5 can be overwhelming, but it is important to hold onto hope. The journey often begins with recognizing symptoms early and never dismissing them as just another ache or pain. Prompt action and the right medical consultation can make all the difference, helping to preserve mobility, independence, and quality of life.
If you or your loved one is experiencing ongoing lower back pain, numbness in the legs, or difficulties with walking and daily activities, do not hesitate. These may be signs that immediate expert attention is needed. Ignoring symptoms or delaying care could put you at risk for additional complications, including irreversible nerve damage. Your health is too important to leave to chance.
Take heart in knowing you are not alone on this path. Physicians dedicated to spine health understand the significance of comprehensive evaluation and personalized treatment plans designed to restore comfort and function. From advanced therapies to compassionate support, the future can be brighter, and every step toward seeking help is a step toward healing.
For expert guidance, compassionate care, and access to the latest treatments for spinal stenosis, request an appointment with Goodman Campbell. They are committed to helping you move beyond pain and return to an active, fulfilling life. Getting back to better can start at Goodman Campbell.


